Not long ago, Alzheimer’s disease could only be formally diagnosed after a person’s death, when a post-mortem examination of the brain revealed the buildup of amyloid plaques and tau tangles – hallmarks of the condition first described by Alois Alzheimer more than a century ago. Thanks to remarkable clinical advances over the past decade, brain scans and blood tests can now reveal the presence of these disease biomarkers in living patients, often long before the emergence of overt symptoms.
While today’s tools can detect the buildup of amyloid and tau in the brain, those changes alone don’t reliably predict who will actually go on to develop dementia – or how quickly their condition will progress.
Now, Stanford researchers have identified a set of proteins in spinal fluid that serve as a kind of molecular signal – also known as a biomarker – that could gauge dementia risk and forecast how a person’s condition may evolve.
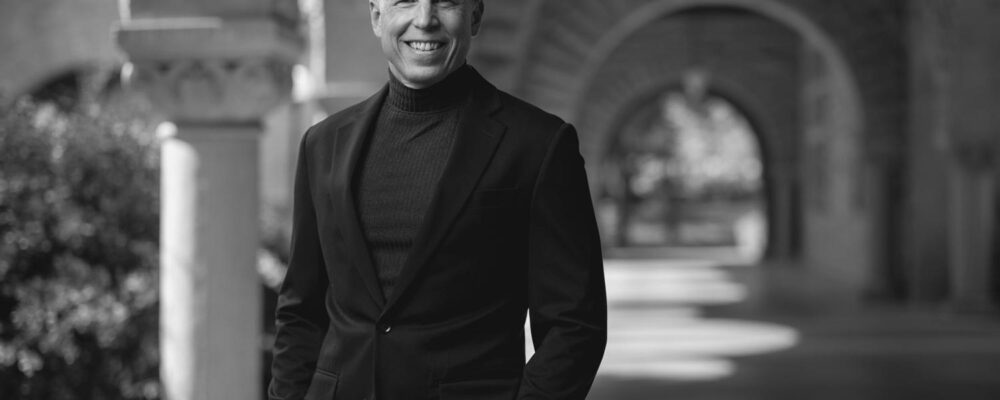
“We found a biomarker that’s independent of the usual signs we see in Alzheimer’s,” said senior author Tony Wyss-Coray, a professor of neurology and neurological science at Stanford Medicine and director of the Knight Initiative for Brain Resilience at Stanford’s Wu Tsai Neurosciences Institute, which supports efforts to understand why some people remain cognitively healthy well into old age.
“Instead, these proteins track more closely with cognitive function and synapse biology,” he said. “That’s what’s new here – and what makes them strong indicators of resilience or decline.”
The proteins Wyss-Coray’s team identified – called YWHAG and NPTX2 – help regulate activity at synapses, the junctions where neurons communicate. These tiny structures are essential for memory and learning but often begin to fail in the early stages of cognitive decline. Unlike traditional biomarker studies, which often rely on the absolute levels of one protein, this analysis revealed that a ratio between two proteins offered a much stronger signal. The ratio of YWHAG to NPTX2 (YWHAG:NPTX2) appears to reflect the brain’s capacity to maintain synaptic connections, offering a new lens on Alzheimer’s disease and brain aging.
If confirmed in future studies, the findings could give doctors a clearer way to assess a person’s risk of cognitive decline – based on a signal tied specifically to mental function rather than just which proteins are building up in the brain. More immediately, the biomarker could make clinical trials more effective by identifying participants who are both at risk of cognitive decline and more likely to benefit from treatment.
The science behind the signal
The research, published March 31, 2025, in Nature Medicine, was led by Hamilton Oh, then a graduate student in Wyss-Coray’s lab, who was on the hunt for a better way to predict Alzheimer’s progression.
As he reviewed the scientific literature, Oh noticed the most commonly used Alzheimer’s biomarkers – amyloid, tau, and neurofilament light – are effective at detecting changes in the brain. But they fall short when it comes to predicting who goes on to develop cognitive symptoms.
“We wondered whether we could find proteins that tracked with peoples’ memory and function – regardless of the pathology in their brains,” Oh said.
Rather than beginning with a hypothesis about which proteins to study, the researchers took an unbiased, data-driven approach. Working with a global network of collaborators, Oh analyzed spinal fluid from more than 3,300 individuals across six major Alzheimer’s research cohorts. Using machine learning, he tested thousands of proteins in different combinations to see which ones best predicted cognitive decline.
The YWHAG:NPTX2 ratio stood out as the strongest signal. The researchers discovered that people with relatively more NPTX2 than YWHAG tended to remain cognitively stable over time, even if they had signs of Alzheimer’s, like elevated amyloid or tau. In contrast, those with a higher proportion of YWHAG were far more likely to decline – and to do so rapidly.
So what do these proteins actually do? That’s still an open question, especially in the case of YWHAG. It’s found throughout the body and in neurons, where it may help regulate brain activity. Mutations in the gene have been linked to epilepsy, suggesting a possible role in neuronal excitability. By contrast, NPTX2 is much better understood. It helps keep neural networks from becoming overactive – something that’s often seen in the early stages of Alzheimer’s disease. Because of this, researchers think NPXT2 may act as a resilience factor: a protein that helps the brain maintain function in the face of disease.
Wyss-Coray believes the new publication is the largest Alzheimer’s study to date that has used proteomics – the large-scale analysis of proteins – to search for biomarkers in spinal fluid. The large dataset allowed the team to identify reproducible signals with greater confidence.
“We can now measure thousands of proteins in a single sample and do it reliably across cohorts from different parts of the world,” he said. “That’s what makes discoveries like this possible – and makes them hold up.”
The data came from several major Alzheimer’s programs at Stanford and beyond, including the Stanford Alzheimer’s Disease Research Center (Stanford ADRC) and the Stanford Aging & Memory Study (SAMS). One of the largest contributions was from the Knight Alzheimer Disease Research Center (Knight-ADRC) at Washington University in St. Louis.
A window into brain resilience
With this new signal in hand, the researchers looked more closely at what it might reveal about Alzheimer’s risk and the brain’s ability to resist cognitive decline.
They found that the YWHAG:NPTX2 ratio begins to rise, predictive of cognitive decline, years before symptoms appear, even in cognitively healthy individuals. In people with inherited mutations that cause early-onset Alzheimer’s disease, the ratio began climbing 20 years before the first signs of memory loss. Even in people without Alzheimer’s, it trended upward with age, possibly reflecting a gradual erosion of synaptic health.
We can now measure thousands of proteins in a single sample and do it reliably across cohorts from different parts of the world. That’s what makes discoveries like this possible – and makes them hold up.”
Tony Wyss-CorayProfessor of Neurology and Neurological Science
This raises a provocative question: Could boosting NPTX2, the protein linked with synaptic health, help preserve cognitive function? In mouse models, boosting NPTX2 appears to protect synapses from damage caused by toxic tau proteins. Delivering it in humans, perhaps through gene therapy, could represent a new frontier in Alzheimer’s treatment.
“If NPTX2 is a resilience factor, restoring it might promote cognitive resilience,” said Wyss-Coray. “That’s a question we’re now excited to pursue.”
Implications for diagnosis and drug development
Encouraged by these findings, the team next looked to see if the same signal could be detected in blood. While the YWHAG:NPTX2 ratio in blood samples wasn’t as predictive of cognitive decline as it had been in spinal fluid samples, the researchers identified a related protein signature that showed more promise. They are now refining this blood-based biomarker with the goal of developing a simpler, more accessible test for brain resilience.
In the meantime, the spinal fluid ratio may have its most immediate use in clinical trials. Alzheimer’s trials often struggle to enroll participants who will reliably develop symptoms within the study period – an important consideration for evaluating if a particular treatment can change that trajectory. A predictive biomarker could improve trial design by identifying those people most likely to decline and most likely to benefit from treatment.
“The primary utility of the cognitive resilience biomarker that we have identified is to make clinical trials much more robust,” said Oh.
The discovery reflects a broader shift in Alzheimer’s research – from detecting damage to predicting, and perhaps even preventing, cognitive decline. And in keeping with the mission of the Knight Initiative, it offers the promise of better understanding – and ultimately promoting – cognitive resilience.
For more information
This story was originally published by the Knight Initiative for Brain Resilience.
“Stanford University, officially Leland Stanford Junior University, is a private research university in Stanford, California. The campus occupies 8,180 acres, among the largest in the United States, and enrols over 17,000 students.”
Please visit the firm link to site